Why does it need better solutions for the treatment of hydrocephalus?
Hydrocephalus, the excess buildup of cerebrospinal fluid in the brain, can affect all age groups. Treatment of hydrocephalus requires surgery and is the leading cause of brain surgery. Since the 1960s, the main surgical strategy is the placement of shunts. However, conventional shunts have very high failure rates [1] and even today the treatment of hydrocephalus is still associated with a high burden for the patients and uncertainty for the treating physicians.
We believe that the current treatment situation for hydrocephalus is not acceptable and better solutions have to be found – effective and reliable hydrocephalus shunts for neurosurgeons to improve the patients’ lives.
Challenges for hydrocephalus shunts
Shunts are life-saving devices but despite long-term experience with shunt implantation and the continuing development of shunt technology they are notorious for high failure rates. [1] Further, conventional shunts fail to address the posture-dependent gravitational effects that influence shunt performance. Overdrainage-related complications can necessitate a variety of different reoperations, which are burdensome for patients and are accompanied by unavoidable perioperative risks.
Learn more about the challenges
Revisions and complications
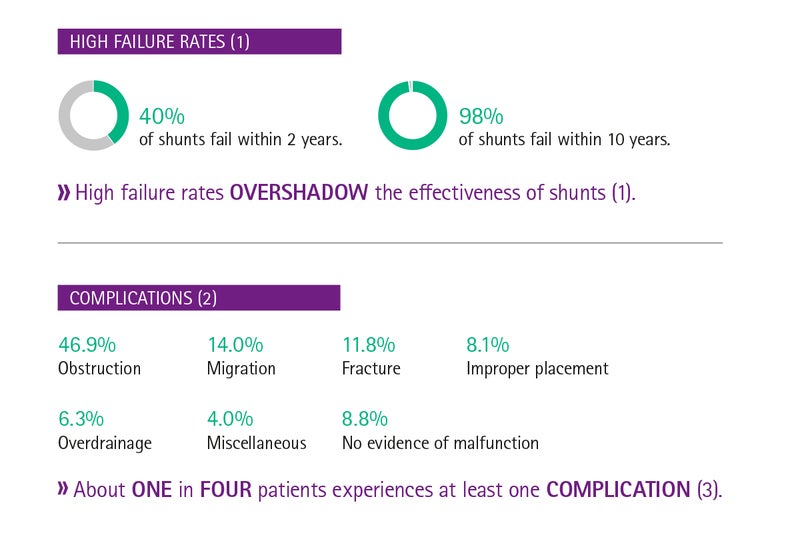
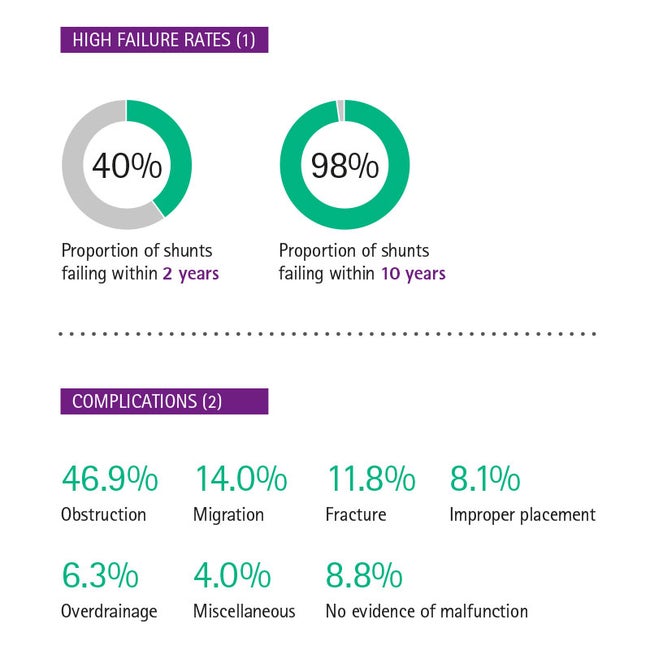
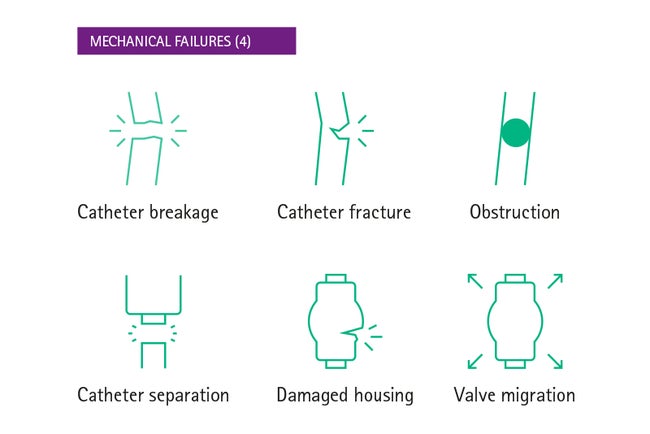
High failure rates continue to overshadow the effectiveness of shunts. [10] It is generally estimated that 40% of shunts fail within 2 years and 98% within 10 years, [1] with no difference between different conventional valves [11] and programmable valves. [12] Nearly every fourth patient is affected by complications, and little improvement in reducing these complications has been made. [13] The most common cause for mechanical complications is obstruction of valve or catheters [14] but a relatively high frequency of non-traumatic subdural hematoma, a potential complication of overdrainage, has also been reported. [13]
Mechanical failure
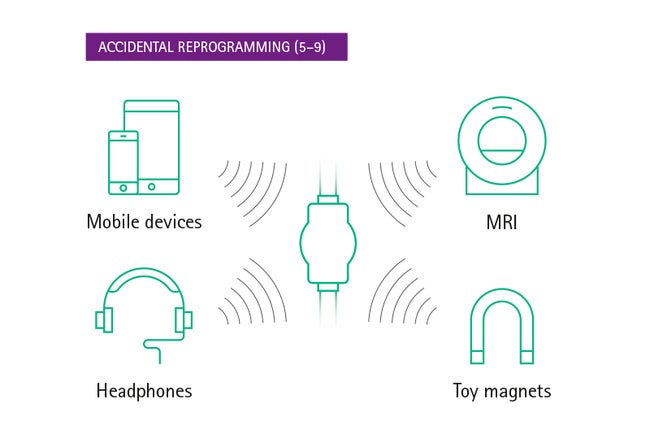
Accidental reprogramming
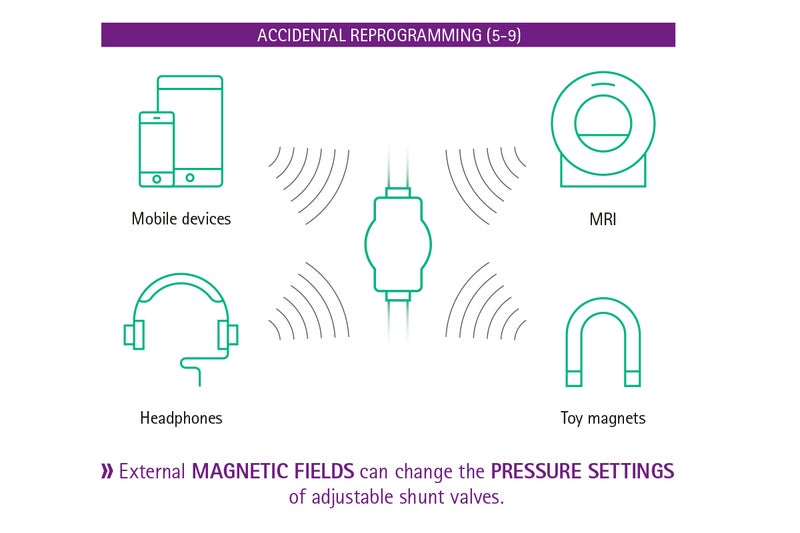
Pressure settings of adjustable valves can be reprogrammed by low-intensity magnetics fields, which are ubiquitous in today’s environment. Smartphones, [5] headphones, [6] tablet devices [7] and even toy magnets [8], [9] have been shown to change the pressure settings of adjustable shunt valves.
The optimal pressure setting of the adjustable valves is of great importance for the patient. Therefore, it comes as no surprise that the possibility of accidental valve adjustments in everyday life is a cause of concern and leads to great uncertainty among patients and doctors alike.
No two patients are alike
When choosing valves it is important to select the type of valve individually in each patient according to the type of hydrocephalus as well as the anticipated postoperative management needs. [9]
Are patients getting optimal individual treatment?
Patients differ with respect to the effective hydrostatic pressure difference between the ventricular system and the abdominal cavity, the major driving force of overdrainage, and also with respect to the intra-abdominal pressure. The selection of the optimal opening pressure of the valve is complex, hence the potential for patient-valve mismatches.
Necessary corrections of patient-valve mismatches, overdrainage-related complications, and high rates of shunt revision require time-consuming follow-up examinations and reoperations, which are burdensome for patients and are inevitably associated with perioperative risks. They also put an additional strain on the already limited time of physicians and surgeons, who are already under stress because of an ever-increasing workload [17] and limited consultation time. [18]
Are conventional adjustable valves the best available therapy?
Treatment with conventional adjustable valves always means finding a compromise:
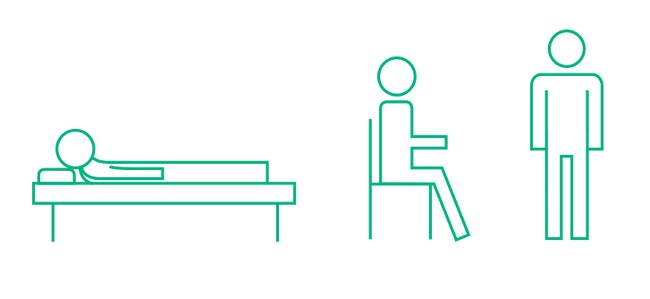
- Lowering the opening pressure in order to achieve a better patient outcome bears the risk of overdrainage while sitting or standing.
- The effect of gravity in the upright position is often the cause of typical overdrainage complications such as hygroma and subdural bleeding, which may lead to severe headaches and nausea.
- An adaption of valve pressure towards higher pressures for compensating overdrainage symptoms can lead to underdrainage in the supine position.
The opening pressure often needs to be adjusted multiple times until an adequate compromise between upright and supine position. The opening pressure often needs to be adjusted multiple times until an adequate compromise between upright and supine position for the individual patient is found. However, patients can never benefit from optimal opening pressures for both the supine and upright position.
What could be better?
Despite the many individual patient factors, there is one thing that is 100% certain: All active patients are exposed to the effects of gravity on cerebrospinal fluid drainage when standing. And not only for a few hours a day, but up to 16 hours – every day. Overcoming this posture-dependent gravitational effect may help to prevent overdrainage and improve patient outcomes.
Get confident! With gravitational shunts.
Gravitational shunts provide neurosurgeons with a possibility to address the posture-dependent effects of gravity, with good clinical outcomes for the patient and a significant reduction of overdrainage events. [19]
Related documents
[1] Lutz BR, Venkataraman P, Browd SR. New and improved ways to treat hydrocephalus: Pursuit of a smart shunt. Surg Neurol Int 2013;4(Suppl 1):S38-50.
[2] Beuriat PA, Puget S, Cinalli G et al. Hydrocephalus treatment in children: long-term outcome in 975 consecutive patients. J Neurosurg Pediatr 2017 20:10-18
[3] Merkler AE, Ch‘ang J, Parker WE, Murthy SB, Kamel H. The Rate of Complications after Ventriculoperitoneal Shunt Surgery. World Neurosurg 2017 98:654-658
[4] Browd SR., Ragel BT., Gottfried ON. and Kestle JR. Failure of cerebrospinal fluid shunts: part I: Obstruction and mechanical failure. Pediatr Neurol 2006 34(2): 83-92
[5] Ozturk S, Cakin H, Kurtuldu H, Kocak O, Erol FS, Kaplan M. Smartphones and Programmable Shunts: Are These Indispensable Phones Safe and Smart? World Neurosurg 2017 102:518-525
[6] Spader HS, Ratanaprasatporn L, Morrison JF, Grossberg JA, Cosgrove GR. Programmable shunts and headphones: Are they safe together? J Neurosurg Pediatr 2015 16:402-405
[7] Strahle J, Selzer BJ, Muraszko KM, Garton HJ, Maher CO. Programmable shunt valve affected by exposure to a tablet computer. J Neurosurg Pediatr 2012 10:118-120
[8] Anderson RC, Walker ML, Viner JM, Kestle JR. Adjustment and malfunction of a programmable valve after exposure to toy magnets. Case report. J Neurosurg 2004 101:222-225
[9] Zuzak TJ, Balmer B, Schmidig D, Boltshauser E, Grotzer MA. Magnetic toys: forbidden for pediatric patients with certain programmable shunt valves? Childs Nerv Syst 2009 25:161-164
[10] Freimann FB, Sprung C. Shunting with gravitational valves--can adjustments end the era of revisions for overdrainage-related events?: clinical article. J Neurosurg 2012;117(6):1197-204.
[11] Gutierrez-Murgas Y, Snowden JN. Ventricular shunt infections: immunopathogenesis and clinical management. J Neuroimmunol 2014;276(1-2):1-8.
[12] Drake JM, Kestle JR, Milner R, et al. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 1998;43(2):294-303; discussion -5.
[13] Pollack IF, Albright AL, Adelson PD. A randomized, controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim-Medos Investigator Group. Neurosurgery 1999;45(6):1399-408; discussion 408-11.
[14] Merkler AE, Ch'ang J, Parker WE, et al. The Rate of Complications after Ventriculoperitoneal Shunt Surgery. World Neurosurg 2017;98:654-8.
[15] Chiriac A, Poeata I, Iliescu B. Mechanical failures of ventriculo-peritoneal shunts. Romanian Neurosurgery 2012;XIX(3):226-9.
[16] Woerdeman PA, Cochrane DD. Disruption of silicone valve housing in a Codman Hakim Precision valve with integrated Siphonguard. J Neurosurg Pediatr 2014;13(5):532-5.
[17] Miyake H. Shunt Devices for the Treatment of Adult Hydrocephalus: Recent Progress and Characteristics. Neurol Med Chir (Tokyo) 2016;56(5):274-83.
[18] Powell A, Savin S, Savva N. Physician Workload and Hospital Reimbursement: Overworked Physicians Generate Less Revenue per Patient. Manufacturing & Service Operations Management 2012;14(4):512-28.
[19] Irving G, Neves AL, Dambha-Miller H, et al. International variations in primary care physician consultation time: a systematic review of 67 countries. BMJ Open 2017;7(10):e017902.