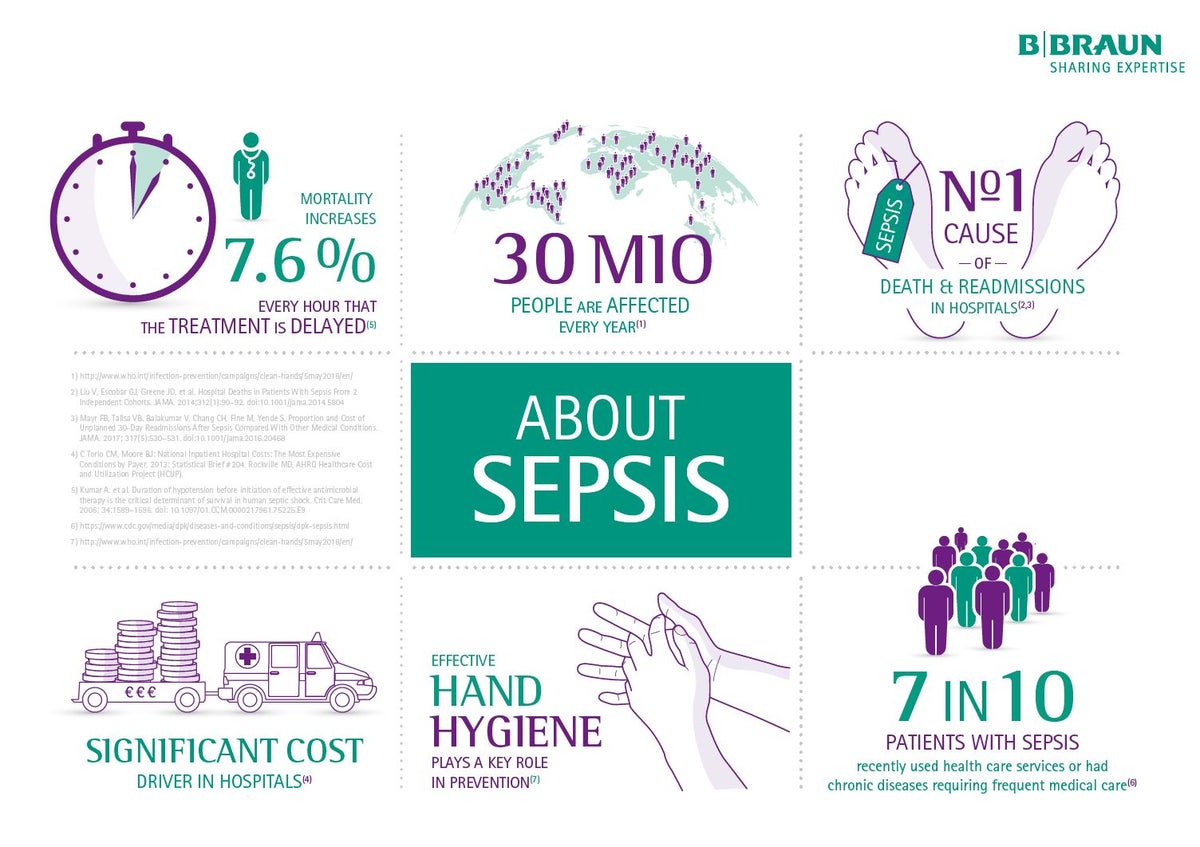
About Sepsis
Health care-associated infections, infections acquired during health care delivery, are common and are a risk factor for developing sepsis but we can prevent this. Effective hand hygiene plays a key role. On world hand hygiene day - 5 May 2018 the focus for everyone should be on prevention of sepsis in health care.
What is Sepsis?
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection. In lay terms, sepsis is a life-threatening condition that arises when the body’s response to an infection injures its own tissues and organs.1
Causes
Sepsis can be triggered by infections caused by bacteria, viruses, fungi, and parasites.2 However, bacterial infections are the most common triggers.
Consequences
Sepsis may lead to shock, multiple organ failure, and death, especially if not recognized early and treated promptly. Between one third and one half of patients with sepsis die.3,4
Many people who survive sepsis recover completely and their lives return to normal. However, as with some other illnesses requiring intensive medical care, some patients have long-term effects.5 These problems may not become apparent for several weeks (post-sepsis), and may include such consequences as:
- Insomnia, difficulty getting to or staying asleep
- Nightmares, vivid hallucinations, panic attacks
- Disabling muscle and joint pains
- Decreased mental (cognitive) functioning
- Loss of self-esteem and self-belief
- Organ dysfunction (kidney failure, lung problems, etc.)
- Loss of hands, arms, legs, or feet (limb amputation)
How to get ahead of sepsis?
Most infections can be avoided by improving hygiene, access to vaccinations and other infection prevention measures. Early recognition of sepsis is crucial to treating patients before their condition worsens and becomes fatal.
B. Braun holistic hand hygiene concept
Infection Prevention Product Range
1) Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810.
2) Munford, Robert S.; Suffredini, Anthony F. (2014). "Ch. 75: Sepsis, Severe Sepsis and Septic Shock". In Bennett, John E.; Dolin, Raphael; Blaser, Martin J. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases (8th ed.). Philadelphia: Elsevier Health Sciences. pp. 91434. ISBN 9780323263733.
3) Engel C, Brunkhorst FM, Bone HG, Brunkhorst R, Gerlach H, Grond S, Gruendling M, Huhle G, Jaschinski U, John S, Mayer K, Oppert M, Olthoff D, Quintel M, Ragaller M, Rossaint R, Stuber F, Weiler N, Welte T, Bogatsch H, Hartog C, Loeffler MReinhart K. Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med, 2007. 33(4): p. 606-18.
4) Kissoon N, Carcillo JA, Espinosa V, Argent A, Devictor D, Madden M, Singhi S, van der Voort E, Latour J. World Federation of Pediatric Intensive Care and Critical Care Societies: Global Sepsis Initiative. Pediatr Crit Care Med, 2011. 12(5): p. 494-503.
5) Widmann CN, Heneka MT. Long-term cerebral consequences of sepsis. Lancet Neurol. 2014;13:630–636. doi: 10.1016/S1474-4422(14)70017-1