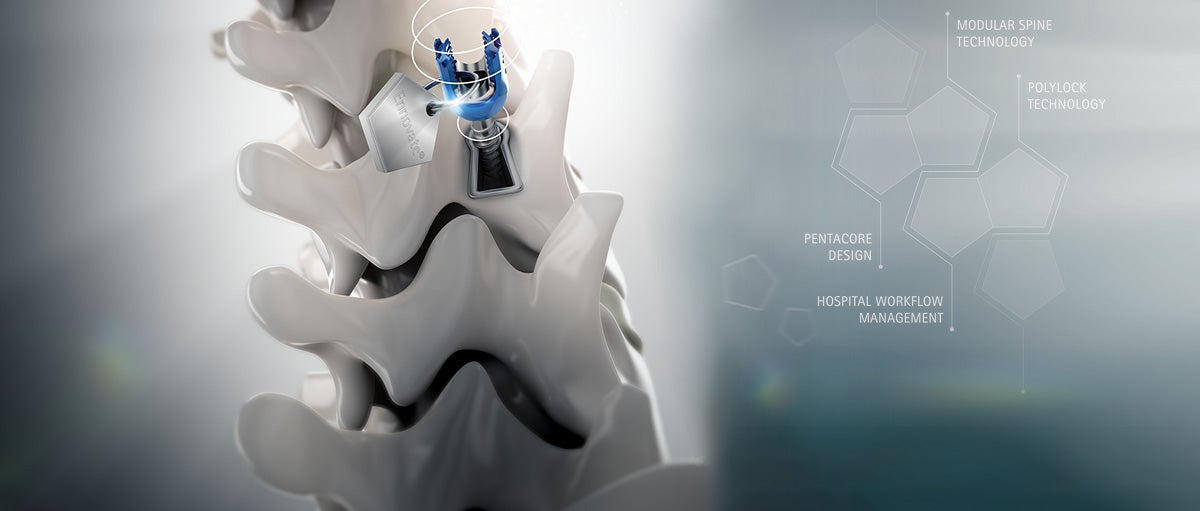
Implant loosening: materials and designs and their impact on bone fusion
Bone ingrowth and osteoconductivity are essential to achieve good fusion of spinal constructs. Titanium alloy 3D cages with porous lattice structures have numerous advantages that may improve results.
Without proper bone fusion, spinal constructs will eventually fail. Factors such as surface structure of the implant, its pore size and porosity, the roughness, as well as the elasticity module of the used material can all positively affect osseointegration (bone ingrowth) and osteoconductivity (the ability of the material to bind certain biological factors that may recruit and regulate osteogenic cells).
Osseointegration and the solid fusion of implant and bone are the most important factors in the “secondary stability” of an implant. By contrast, “primary stability” comes from mechanical engagement with the bone, a high contact surface together with high roughness (and thereby higher friction forces), a structure that allows the partial subsidence of edges or spikes and a good shape fit.
3D cages made from titanium alloy (Ti) with a 3D lattice structure and a rough surface offer a number of advantages regarding both osseointegration and osteoconductivity.
Learn more about
Materials: titanium alloy allows bone ingrowth and promotes stability
The titanium alloy Ti6AI4V ELI is a widely accepted and biocompatible material for implants. The biocompatibility of titanium means that osteocytes can start bone growth directly on and into the material, helping to stabilize the implant. By contrast, cages made purely from polyetheretherketone (PEEK) have no connection to bone, as bone does not directly bond with PEEK; a PEEK implant is always separated from bone by a fibrous tissue layer. Therefore, pure PEEK cages by themselves offer neither primary nor secondary stability. In these cases, the stability is derived from bone growing around the cage. All cages – irrespective of material – should be implemented with a posterior fixator (plates or pedicle screws), which can increase stress shielding that in turn may lead to pseudarthrosis.
Young’s modulus (elasticity module) close to that of cortical bone
Solid titanium alloy Ti6Al4V ELI has an elasticity module of around 110 GPa, much higher than the 5-20 GPa of cortical bone. However, the lattice structure of the Aesculap 3D cages was shown to have a Young’s modulus far closer to that of cortical bone, improving bone tissue growth. [1] (It should also be noted that elasticity module values established in studies are mainly due to tests of tensile strength on solid material, while the stress on lattice-structured cages is mainly due to compression force.)
Lattice structure and compressive strength
The 3D lattice structure of the cages combines an elasticity module similar to bone with a high compressive strength; the compressive strength of the 3D lattice structure is actually even higher than the median bone strength reported in studies. [2] In addition, the 3D lattice structure achieves a higher compressive strength than PEEK. [3]
Better bone ingrowth and stability due to porosity, pore shape and size
Ti6AI4V ELI 3D cages are designed to match the porosity of normal bone, which increases bone attraction and bone ingrowth into the cage; studies have shown that an implant’s stability after implantation depends on the pore shape and size of the implant surface facing the host bone. [4] The median pore size of 900μm and the porosity of 50 to 55 percent is consistent with that of cancellous bone; both pore size and porosity are within a range that favors bone ingrowth. According to the average pore size and porosity of cancellous bone (approximately 1 mm / 50-90 %), the 3D lattice structure Structan® features an all-over regular pore size of 900 μm as well as a mean interconnected porosity of 50-55 %. [5] Pore size and porosity are in a favorable range to stimulate bone in-growth. [6], [7]
Other studies have confirmed the high bone-implant contact throughout porous implants (vs. solid implants) and the significance of a pore size > 300μm due to enhanced new bone formation and formation of capillaries. [8], [9], [10]
Summary
Ti6AI4V ELI 3D cages are designed for bone ingrowth and osteoconductivity to achieve good, long-term fusion of spinal implants.
[1] Brizuela A, Herrero-Climent M, Rios-Carrasco E, Rios-Santos JV, Pérez RA, Manero JM et al. Influence of the Elastic Modulus on the Osseointegration of Dental Implants. Materials 2019;12(6):980.
[2] Azami M, Moztarzadeh F, Tahriri M. Preparation, characterization and mechanical properties of controlled porous gelatin/hydroxyapatite nanocomposite through layer solvent
casting combined with freeze-drying and lamination techniques. Journal of Porous Materials 2010;17:313-320.
[3] Rae PJ, Brown EN, Orler EB. The mechanical properties of poly (ether-ether-ketone)(PEEK) with emphasis on the large compressive strain response. Polymer 2007;48(2):598-615.4.
[4] Mahmoud D, Elbestawi M. A. Selective laser melting of porosity graded lattice structures for bone implants. The International Journal of Advanced Manufacturing Technology 2019;100(9-12):2915-2927.
[5] Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaf-folds and osteogenesis. Biomaterials. 2005;26(27):5474-91.
[6] Taniguchi N, et al. Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Materials Science and Engineering: C. 2016;59:690-701.
[7] Van Bael S, et al. The effect of pore geometry on the in vitro biological behavior of human periosteum-derived cells seeded on selective laser-melted Ti6Al4V bone scaffolds. Acta biomaterialia. 2012;8(7):2824-34.7.
[8] Bobyn JD, Pilliar RM, Cameron HU, Weatherly GC. The optimum pore size for the fixation of porous-surfaced metal implants by the ingrowth of bone. Clin Orthop Relat Res. 1980;150:263-270.
[9] Palmquist A, Snis A, Emanuelsson L, Browne M, Thomsen P. J Long-term biocompatibility and osseointegration of electron beam melted, free-form-fabricated solid and porous titanium alloy: experimental studies in sheep. Biomater Appl 2013;27:1003-1016.
[10] Mahmoud, Dalia; Elbestawi, M. A. Selective laser melting of porosity graded lattice structures for bone implants. The International Journal of Advanced Manufacturing Technology, 2019, 100. Jg., Nr. 9-12, S. 2915-2927.